There are changes that need to be made in our health care communities: physicians and complementary health practitioners must collaborate; patients must take responsibility for their health; doctors need to approach wellness creatively; and, creatively dialoguing. On-going communication and support among all practitioners and patients is crucial in closing the wellness loop. To facilitate these changes, we need to focus on the three R's referral, retention and reporting.
Before we take a closer look at these three R's, several questions need to be answered that will later be addressed in this article. They are: "How does a patient navigate the wide medical options that are now available after an initial medical diagnosis? How does that patient seek out a physical therapist, a chiropractic physician or a personal fitness professional? What type of referral, retention and reporting plan successfully addresses, motivates and ultimately meets a patient's health expectations?"
To answer these questions, I interviewed three practitioners in their respective fields Dr. Alan Falkoff, MD, DABFP; Dr. Heather Gansel, DC, a chiropractic physician; and Jinger
Marilyn Gansel: I would like to start with your definition of wellness, since the term is often loosely defined or ambiguous.
Alan Falkoff: I see wellness as an all-encompassing approach to healing. It incorporates the medical but also the physical or mental well-being of the individual. Wellness gives a person control over their life. As a physician, I exam patients by means of physical tests to determine risk factors, but if my patients have psychological problems or if they need to lose weight, their health condition or mental state can affect their longevity. I try to educate my patients with regard to their risk factors, offer them alternatives so they can take control over their lives. If that means they need to increase their self-confidence, I advise them to seek counsel; if they need to lose weight, I encourage exercise, which also releases natural endorphins and can help with other symptoms such as depression. I believe that healing occurs when the mind, body and spirit are in concert.
Heather Gansel: I agree with you, Alan. I see wellness as the whole body being able to synergistically work as one. Wellness is a best seen as a triangle with the physical, mental and spiritual components all connected so the individual feels a sense of overall peace.
Jinger Berry: Our Health & Fitness Institute is a place that incorporates many different types of exercise programs and nutritional classes to maintain a healthy life. Our goal is the reduction of health risks and overcoming the symptoms and effects of chronic medical conditions. So, wellness for us means incorporating the types of programs and other services that give people the opportunity for a healthier lifestyle.
MG: While each of your wellness facilities is structured differently Alan's and Heather's are more like hospital outreach centers while Jinger's institute is located within a hospital you have captured the same essence of wellness in your definitions. How do you or your facility generate referrals to other health care and fitness professionals?
AF: I like to think of myself, the general practitioner, as the "search engine." When a patient comes to me, I do an initial assessment of his needs. The tests performed are, of course, based on that patient's current health, genetic make-up and age. After the results of the tests are analyzed, red flags may pop up, and I am able to prescribe other tests, medicines and/or referrals to other specialists or alternative care providers. Each patient is an individual so their prescription plan is unique for them. Their plan depends on their individual risk factors. Ultimately, I want them to take control of their lives.
HG: When I look at a patient, I try to determine precisely what condition, ailment, disease or illness they are suffering from or experiencing. I assess each individual case and then co-manage their care with other professionals in various fields to give the individual the opportunity for optimal health and wellness. We also try to involve the patient by having that person see all the possibilities for healing rather than just focusing on the problems he may be experiencing.
JB: Since I am not a physician but an exercise physiologist, I work along side other physicians, alternative care professionals and physical therapists in designing exercise programs and nutritional seminars that will help individuals focus on a heath care plan as well as also educating the community on many health-related topics.
MG: So, from what I understand in your practice/wellness center, Alan and Heather, patients come to you first for a physical exam before moving on to other practitioners or professionals. And, instead of acting as the "expert," you see yourself more as a collaborator.
AF & HG: Yes.
MG: For you, Jinger, patients come to your facility and use your services after their medical condition has been evaluated ' or tested by an outside physician or health care practitioner and then you provide exercise programs and rehabilitation, when necessary, as a way for them to begin their healing process.
JB: That's correct.
MG: How specific do you get with referrals? How exactly does that process work? Would you suggest to a patient that an acupuncturist, a massage therapist, a psychiatrist, a chiropractor, a physical therapist and/or a personal trainer be part of the healing progression?
AF: It really all depends on an individual's needs. For example, I do not prescribe a massage therapist for a diabetic or a person suffering from sleep apnea. But I would prescribe massage as part of the healing process for a patient who is stressed or for a person who feels that acupuncture is helpful in their cure, I would recommend and refer them to a skilled acupuncturist. Realizing that I am not a specialist in everything for example, I can't rehab a shoulder injury nor can I sit down and prescribe how many calories my patient should be eating or what she should eat to lose weight I welcome the collaboration between conventional and alternative medicine. I would rather have my patient work with a competent physical therapist, a chiropractic physician or a licensed nutritionist so that my patient can reap long-term benefits.
HG: I agree with you, Alan. Earlier you said you see yourself as the "search engine" looking for the diagnosis. I see myself, the chiropractic physician, as the "gatekeeper" an alternative, preventive care-giver. I have a vast knowledge of other fields of medicine. Like you, I also perform a physical exam and determine a patient's medical condition; the results of which, then prompt me to refer my patient to a personal trainer, ophthalmologist, cardiologist, physical therapist, nutritionist or any other conventional or alternative care provider. To whom I refer each patient really depends on what is going on in their systems at that time. As the "gatekeeper," I cannot be the "be-all" for every patient. Like you implied, Alan, as a physician you have to recognize what is out of your scope. You need to listen closely to what your patient says in the first assessment or physical exam and then send them to the physician or healer who can help them best.
MG: Obviously, you all see that a collaborative, mentorship effort is needed by all members of the medical and alternative care community to reach the client's optimal health needs.
HG: Yes. From my experience, we cannot set a limitation on how or why healing happens. Physicians and complementary health care professional must respect each profession and utilize that knowledge to help the patient.
JB: The most important point here is that we must build solid relationships with each other and our patients or clients.
MG: Do you or does your office/facility offer wellness seminars; for example, smoking cessation, healthy eating, dealing with diabetes, back care, stress management and/or refer patients to support groups?
JB: We are so proud of the programs and seminars we have developed and offer to the community. First, we have a 12-week exercise program that every new member of our center has the opportunity to try. Each program varies according to the needs of that person. But the patient/client has the opportunity to meet with a personal trainer after the guidelines for the exercise program are set by one of our exercise physiologists. Some programs include resistance training; others, aquatic classes, ball therapy classes, yoga and meditation or total body conditioning. Our goal is to provide monthly educational seminars. We have seminars on weight loss, depression and ski and golf injury prevention, pain management and more. We are thrilled to be currently offering a free obesity clinic for teens. Through community donations and funding, we have a 12-week program for teens that includes nutritional guidance, exercise programs and psychological help.
AF: We offer continued nutritional seminars every several months. Soon, we are planning larger seminars for the community at local hotels where we will be inviting guest speakers, such as nutritionists, exercise physiologists and chiropractors.
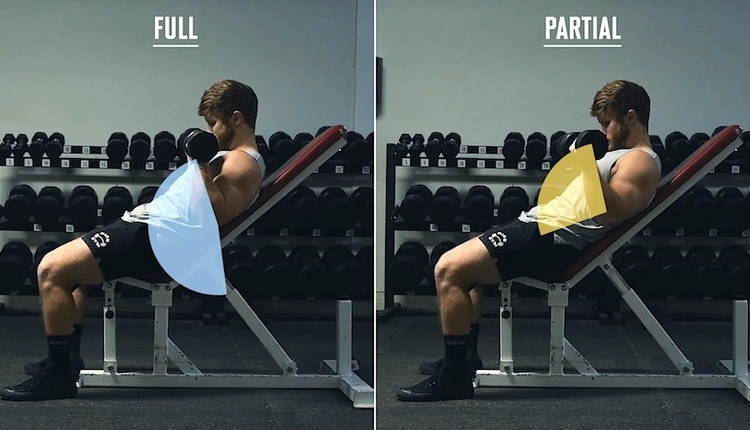
HG: We also believe in educating people so they have a better understanding of their medical condition. I enjoy lecturing on back care, as well as on rehab support. For example, I see so many patients with shoulder pain. I like to demonstrate simple exercises that they can do at home or when traveling to strengthen the shoulder girdle. So, often we design our seminars for clients/patients to act as participants rather than sit through a talk on stressful eating behaviors.
JB: We also offer patients opportunities to attend workshops where, for example, they can actually cook healthy meals under the guidance of a dietician. '
MG: That's great! You all seem to be doing an excellent job of referring and educating patients. Let's talk about retaining the patient or keeping them on track. How do you communicate with each other regarding the patient's medical diagnosis and then share that information with the patient?
AF: We email each other; write lengthy summaries on client/patient diagnosis and health changes. Forms are sent out; for example, I might send a form/summary to my patient's cardiologist. This summary includes a recommendation for my patient's health; a copy of which goes to my patient. Once a month, we have a meeting with the principals involved in a patient's care especially, in a more difficult case. If there is a medical condition that is out of the ordinary, we need, as a group, to decide what might work better.
HG: I also have a form that I designed. It is really a patient update form and I send out a letter to the person to whom I referred my patient. I gather information from each doctor or alternative care provider and we talk frequently on the phone. Each time I meet with my patient, I discuss their progress, making phone calls in between to find out how she/he is doing and to answer any questions.
JB: We keep in contact with each other pretty much through email, phone calls and reports. Since we follow-up with our clients every 30, 60 and 90 days, we feel we have a pretty good pulse on how they are doing. Again, if our client's health changes for better or worse we have an extensive referral system to support the client's needs.
MG: Does all of the emailing, phone calling and report writing take a lot of coordinating? How do you keep the patient coming back how do you keep him on track and monitor his progress? And, does the patient have a role in all this? What responsibility does the patient need to take to use all of the services of a wellness center?
JB: The toughest part is following up with people. We feel the onus is on the person. But we also need to promote the message that they need our services, that they can do this! One way we try to monitor and track our patients is by utilizing a computerized machine called Fitlinxx. These machines are attached to our exercise equipment providing our patients with instant access to their workout programs and their progress. In addition, all the exercise machines are networked into a central database, giving staff access to a wealth of information on an individual's progress. We also are able to learn the last time an individual worked out; and we can send reminder postcards as a follow-up to absent persons encouraging them to return.
AF: The patient is fully responsible to make her life better and regain control of her life. We strive to motivate patients so they will be successful. By building a support team and showing the patient that he is making progress his cholesterol is better, his clothes are fitting better, he is starting to date again, he is on less medication the results of which are structuring an independence to lead a healthier lifestyle. Patients cannot see failure. We need to reward our patients, give them positive strokes. They have to see that their body fat has changed for the better; that they look and feel better.
HG: I think that both the medical community and the patient are responsible. The patient has to realize that his case consists of multiple healing levels and doctors need to educate patients about the fact that his medical condition may consist of multiple levels of care. Then patients will experience change and wellness.
MG: I also believe that when physicians and complementary health care practitioners focus on solutions, options and possibilities rather than on patient problems, patients will take responsibility for their health. When patients use the services of medically supervised professionals that address the many facets of their health issues, their lives will be filled with hope and healing. I believe that we can close the wellness loop as we work together and integrate our treatment plans. A strong referral system, good retention procedures and constant reporting among professionals and their patients/clients will keep individuals focused on preventive health care. imagine that this is what you and your centers are attempting to do and I applaud your efforts. Thank you for your hard work and your thoughts on closing the wellness loop.
Marilyn Gansel is the founder and owner of Fitness Matters Inc. She is certified by ACE and the Aquatic Exercise Association. She holds specialty certifications for seniors and youth, pre and post natal. Marilyn regularly consults with fitness and health professionals in developing their own fitness studios and wellness centers. For more information, please visit their Web site at www.fitnessmatters.com.