Working with breast cancer patients is a valuable experience; an in-depth understanding and specialized training of common side-effects, physical implications and comorbidities is critical prior to training patients. The most common issues that plague post-mastectomy patients are upper-crossed syndrome and range of motion limitations in the affected shoulder.
As a result of these postural deviations, mastectomy, lymph node dissection, and/or radiation, the chest muscles may become tight, shortened and spastic. This not only exacerbates the postural deviations, but may limit the ability of the patient to move their arm/shoulder through flexion, extension, abduction and external rotation. While this is a general statement, the majority of patients will present these symptoms. This is compounded if the woman undergoes reconstructive surgery. Not only will it further exacerbate upper-crossed syndrome, it will create a muscle imbalance in the area of surgery if either the rectus abdominis or latissimus muscle are used for reconstruction.
The most important factor in the safety and efficacy of the exercise program is the initial assessment. At the very least this should include a comprehensive postural assessment as well as shoulder range of motion measurements taken with a goniometer. By selecting the wrong combinations of exercises, the results may not only be undesirable, they may in fact be detrimental.
For example, if a client presents with moderate to severe upper-crossed syndrome, performing any kind of “pushing” exercise that would involve the chest muscles (chest press), could worsen the syndrome by causing the pectoral muscles to tighten and contract. Instead, the goal needs to be stretching the chest wall and strengthening the opposing muscles in the back; particularly the scapular stabilizers.
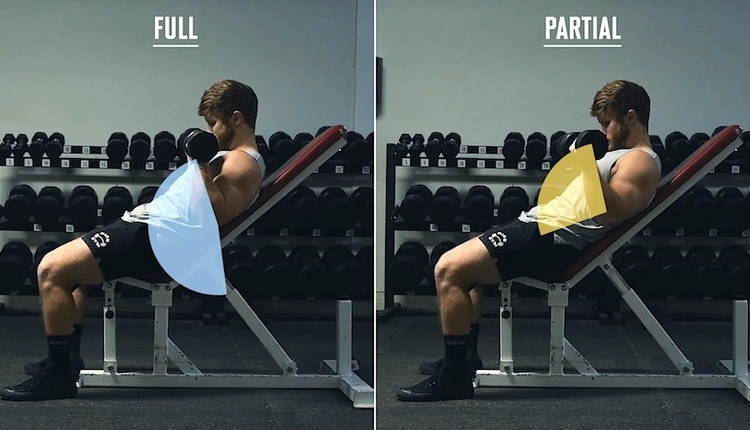
Prior to adding load (resistance) of any kind, the patient should have close to full range of motion through the particular plane. Without correcting the range of motion first, the patient will reinforce the negative movement pattern by performing strength training exercises through a limited pattern of movement. Therefore, the initial focus should be on range of motion exercises. These may include very basic exercises that the patient can do on their own; front wall walks, side wall walks, pendulum swings and corner stretch.
Once close to full range of motion is achieved, the emphasis can be on strength training. Not only will this help to correct the postural and range of motion deviations, it will help increase bone density and lean muscle mass. Many women will either be of menopausal age or thrown into menopause from their cancer treatment. With estrogen no longer being produced, the risk of osteoporosis increases. Furthermore, the long-term side-effects of chemotherapy include osteoporosis, diabetes and damage to the heart and lungs, all of which can be avoided or improved through proper exercise recommendations.
The last part of the equation is the risk of lymphedema of the affected arm/shoulder. Lymphedema is the swelling of the extremity following the removal of, or radiation to, the lymph nodes on that side. Lymphedema is progressive if untreated and can be very painful and disfiguring. It can happen at any time after surgery; one hour or 50 years. The risk doesn’t increase or decrease with time, however a higher percentage of body fat, infection, age and poor nutrition can all increase the risk once someone is at risk. Following lymph node dissection and/or radiation, the lymphatic pathways do not operate with the same efficacy as they did previously.
Therefore, we no longer know the individual’s exercise threshold. It is critical to start and progress slowly. This allows for a gradual increase in exercise frequency, intensity and duration. If at any point there is swelling, advise the patient to stop exercising and see their doctor immediately to determine if, in fact, they have the onset of lymphedema.
A typical exercise session should begin with cardiovascular exercise. This, too, should be gradually increased at a rate with which the client is comfortable and to which their body responds favorably. Following the warm-up they should be instructed to do a series of lymph drainage exercises to open up the lymphatic pathways and prepare the body for exercise. Then determine the areas of “need.” Once they have close to normal range of motion, the goal becomes strength training and choosing exercises that will strengthen the weaker muscles and stretch the tight and shortened muscles. Weight/resistance should be very gradually increased and attention paid to any potential swelling of the extremity. If they have undergone reconstruction, focus on correcting muscle imbalances ensuing from amputation.
Choose your exercises carefully. No two breast cancer patients are the same. Not only are you taking into consideration their surgery, reconstruction and treatment, you have to also factor in comorbidities. Anyone who wants to work with cancer patients should undergo specialized training. It is very complex and the untrained professional can end up doing more harm than good.